Diagnosis of Aortic Stenosis
Aortic stenosis can be diagnosed after detailed patient history, physical examination, and echocardiography performed by specialist cardiac sonographers. Aortic stenosis should be considered if patients exhibit the classic signs of:
- Breathlessness on exertion
- Angina / chest pain on exertion
- Syncope / pre-syncope
- Heart failure
In the below video, Interventional Cardiologist Dr Mark Webster explains the common symptoms patients may present with where aortic stenosis could be the underlying problem. This includes if, “their exercise capacity has reduced, if they develop chest tightness with exertion, breathlessness with exertion, or dizziness with exertion.”
A chest x-ray showing signs of an enlarged heart (cardiomegaly) may confirm a suspicion of left ventricular (LF) systolic failure. Other non-specific findings on a chest x-ray may be:
- calcification of the aortic valve,
- pulmonary congestion, and
- post-stenotic dilation of the aorta.
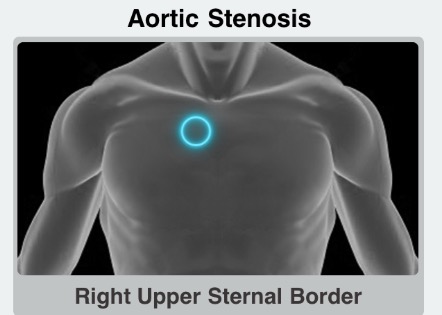
A patient with aortic stenosis may also have a systolic, “crescendo-decrescendo” murmur that may be heard at the right sternal border, in the second intercostal space. This murmur may radiate into the carotid arteries bilaterally, which is usually heard best when sitting the patient upright. The loudness of the murmur does not equate to the severity of the disease.
Left Ventricular Hypertrophy (LVH) may be present in a 12 lead ECG. Which would usually present as tall R waves in V5-6 and deep S waves in V1-2. However, it is well recognised that these ECG changes may not be present in many patients with aortic stenosis1.
Echocardiography and Aortic Stenosis
Echocardiography (Echo) is the definitive diagnostic test for aortic stenosis. These tests are readily available but require highly specialised sonographer skills to elicit an accurate diagnosis. Early referral for an Echo should be considered in patients suspected to have aortic stenosis.
Dr David Smyth, Interventional Cardiologist, discusses below the role of an ECG (Electrocardiogram) in the diagnosis of aortic stenosis. Further explaining the other indications that might be evident during the ECG, including “fibrosis, heart block… or potentially requiring a pacemaker following a surgical or transcatheter intervention.”
The severity of aortic stenosis is determined by measuring the aortic valve area (AVA) and calculating the pressure gradient between the LV and the aorta on echocardiography. These acquired measurements will determine the severity of aortic stenosis, mild, moderate, or severe.
| Mean Gradient (mmHg) | Aortic Valve Area (cm2) | |
|---|---|---|
| Mild | 15-25 | >1.5 |
| Moderate | 25-40 | 1.0-1.5 |
| Severe | >40 | 0.7-1.0 |
| Critical | N/A | <0.7 |
A two-dimensional echocardiography procedure can demonstrate a thickened aortic valve, reduced leaflet mobility, and concentric left ventricular hypertrophy. To quantify the severity of the condition, a Doppler examination can be used by measuring the pressure gradient across the aortic valve and in calculating the aortic valve area (AVA). The velocity of blood flow across the aortic valve, as determined by a continuous-wave Doppler, is used to calculate the transaortic pressure gradient2.
Whilst access to Echo is readily available, it is recommended that specialist cardiac sonographers perform the examination due to the highly technical nature of these scans to illicit accurate readings and measurements.
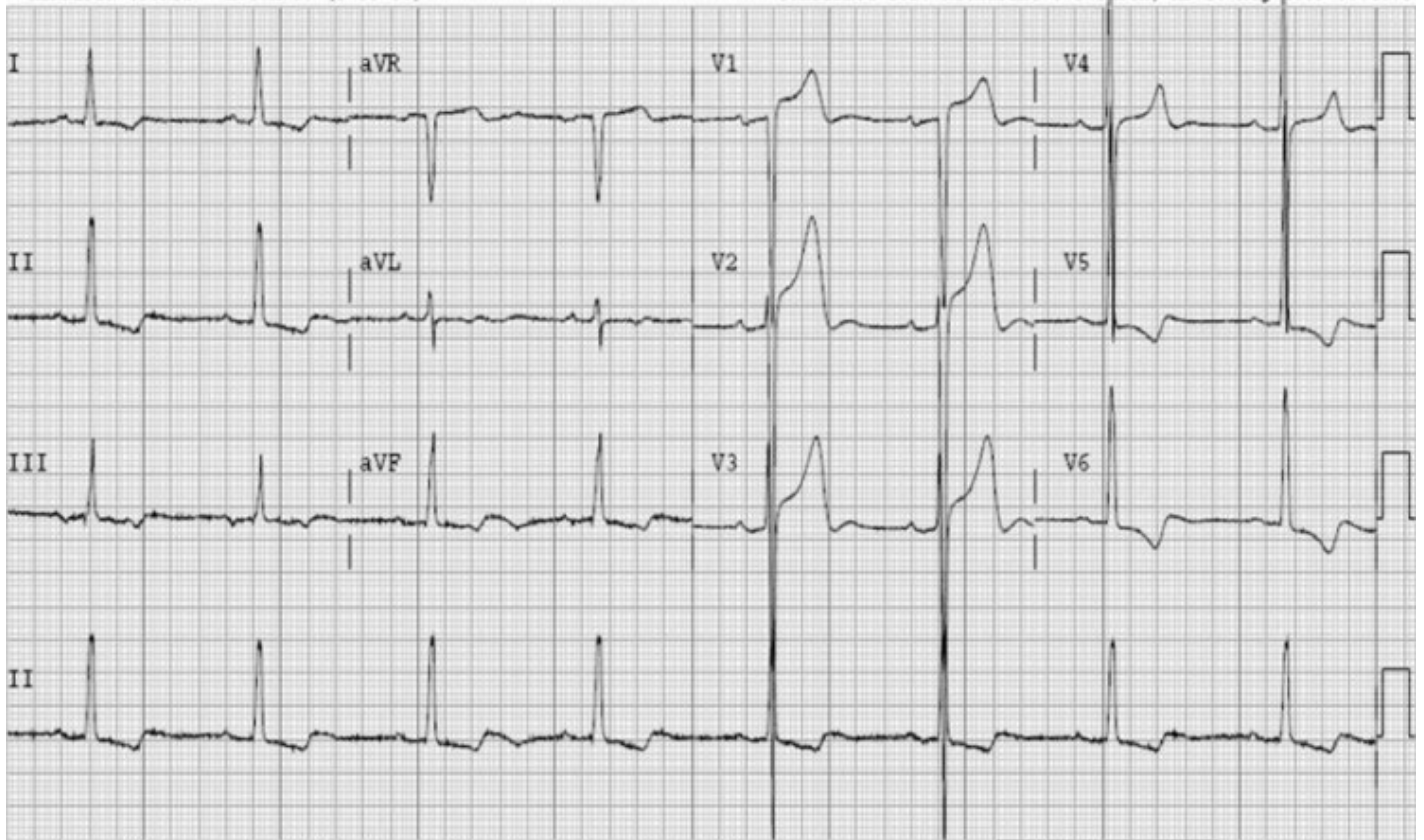
Image 1: Example of a 12 lead ECG showing left ventricular hypertrophy3
Aortic Stenosis and Heart Sounds
Listening for an aortic stenosis murmur is an important step in ruling out if a patient has aortic stenosis. Watch the video below for a description of the sound of an aortic stenosis murmur by Associate Professor Gerald Wilkins.
Auscultation of the heart in patients with aortic stenosis is critical to aid in the diagnosis of the disease. As the blood is ejected from the narrowed aortic valve during systole, it is possible to hear a distinct murmur. The typical murmur of aortic stenosis is described as a high-pitched, “diamond-shaped” crescendo-decrescendo, mid-systolic murmur. The ideal location to listen to this murmur is near the right sternal border, second intercostal space. The murmur may radiate into the neck and carotid arteries.
In mild aortic stenosis, the murmur peaks in early systole. However, as the disease progresses the peak moves to later in systole as a longer time is required to complete LV systole, and aortic valve closure is delayed. The intensity of the murmur typically increases as disease progresses; however, when heart failure develops and cardiac output declines, the murmur often becomes softer. Thus, the intensity of the murmur is not a good indicator of disease severity.
Listen to an Aortic Stenosis Heart Murmur
(To hear the heart sounds clearly, we recommend using your headphones)
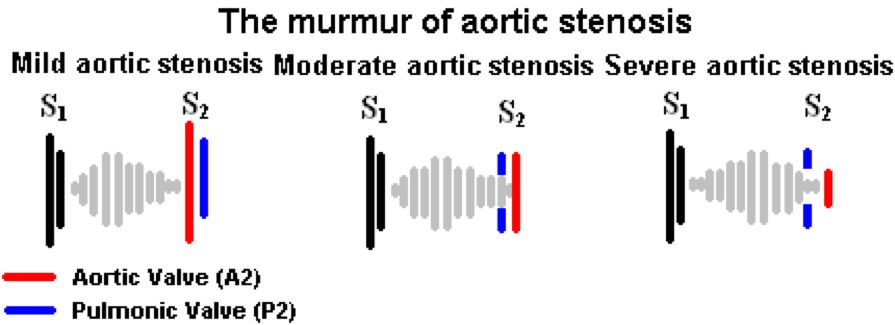
Image 1: A murmur of Aortic Stenosis4
Where to Hear an Aortic Stenosis Heart Murmur
Pictured below is the ideal location to hear typical aortic stenosis murmur. Right sternal border, second intercostal space5.
Patient Disclaimer: All content on the Hope For Hearts site is created and published online for general information purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Please see your doctor if you have any questions or concerns.
- Seiler C, Jenni R. Severe aortic stenosis without left ventricular hypertrophy: prevalence, predictors, and short-term follow up after aortic valve replacement. Heart (1996); 76(3): 250-5.
- Healio - Learn The Heart
- Life In The Fast Lane - ECG Library Diagnosis
- GPOnline
- iMedicalApps
