Treatment of Aortic Stenosis
Aortic stenosis is a mechanical problem that requires a mechanical solution in order to treat the affected valve. Early referral of patients with signs and symptoms of moderate to severe aortic stenosis will allow treating specialists to decide on the most appropriate course of intervention for each patient.
Treatment of aortic stenosis with medications may reduce the impact of symptoms of aortic stenosis but has not yet proven effective in improving outcomes.
There are three main surgical procedures for treating aortic stenosis:
- Surgical aortic valve replacement (SAVR)
- Transcatheter aortic valve implantation (TAVI)
- Balloon valvuloplasty.
Cardiothoracic Surgeon Mr Indran Ramanathan explains, “aortic stenosis is very easily treatable either by surgery or transcatheter route.” He further indicates that in New Zealand, low-risk patients may typically have surgical aortic valve replacement, and high-risk patients may typically receive transcatheter aortic valve implantation.
Types of Valves
Patients with severe aortic valve disease will require aortic valve replacement in order to reduce symptoms of the disease.
The diseased aortic valve is replaced with an artificial valve. There are currently two main types of artificial valves available.
- Mechanical valves- which are currently made from carbon fibre, and
- Biological valves- manufactured from with Bovine (cow) tissue or Porcine (pig) tissue.
Cardiothoracic Surgeon Mr Peter Alison explains the various types of tissue and mechanical valves in the below video, as well as the various ways to approach the aortic valve.
Mechanical valves are extremely durable and very reliable. However, the patient will be required to take a lifelong anticoagulant, such as Warfarin. The patient will also require regular blood tests to monitor their INR levels and potentially have regular medication adjustments to remain within the therapeutic range. Biological valves do not require anticoagulation but are not as durable and have an estimated longevity of between 15-20 years1. A biological valve may require replacement after this time2.
There are also many other considerations around valve selection, and each patient should have a detailed discussion with the surgeon about which type of valve is best suited to their needs.

Image 1: Two types of artificial valves3
Aortic valve replacement is regarded as the definitive therapy for severe aortic stenosis. The multi-disciplinary heart team will conduct a thorough evaluation of the patient’s status and make the final treatment decision for either surgical AVR (SAVR) or transcatheter aortic valve implantation (TAVI).
Pharmacological Considerations for Patients with Aortic Stenosis
Interventional Cardiologist, Dr Krys Milburn explains the pathophysiology of a patient requiring medication for the management of their aortic stenosis. Additionally, he explains the challenges many primary care physicians can have with supplying their patients with the right type and dose of medication.
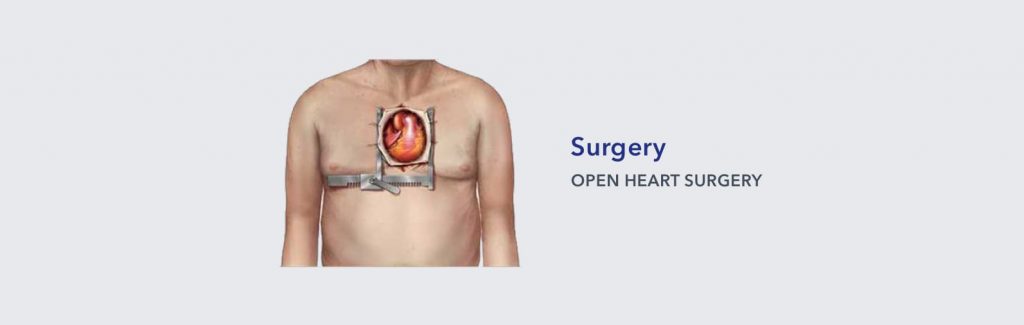
Surgical Aortic Valve Replacement (SAVR)
The primary treatment of aortic stenosis is replacement of the damaged aortic valve. However, many patients are not considered for open surgical valve replacement due to patients having concomitant risk factors and other associated co-morbidities.
Cardiothoracic Surgeon Mr Dominic Parry discusses the benefits of SAVR, the types of valves available and the role of medications.
When a patient requires an open heart procedure, the sternum is divided, and the heart is visualised to allow surgical access to the heart. Once the heart is accessed, patients may be put on a heart-lung machine for the duration of the procedure, while cardiac surgeons replace the aortic valve. Open heart procedures may also allow other surgical interventions to be performed, such as mitral valve repair/replacement and coronary artery bypass grafting. This allows the patient to have one surgical procedure rather than multiple surgeries.
Recovery Period
Recovery from open heart surgery will often be individualised, however, most patients will require ICU admission for a period of time before being transferred to a ward to facilitate post-operative recovery. A full recovery can usually take up to 8 weeks, although this depends on the patient’s pre-existing condition. Many patients are able to drive again whilst recovering, but your surgical team will determine these guidelines individually4.
Does Age Prohibit Treatment Options?
In the video below, Cardiothoracic Surgeon Dr Peter Alison discusses how age contributes to patients receiving treatment and what the results say. He signifies that a patient receiving treatment is likely to yield good results, as improving their quality of life and reducing their mortality is proving to be very achievable.
Transcatheter Aortic Valve Implantation (TAVI)
Transcatheter aortic valve implantation (TAVI) is a treatment option for aortic stenosis patients. For many years, the only treatment option available to aortic stenosis patients was surgical replacement; however many patients were too high risk for this type of treatment. Trials have since revealed that patients who are high risk have proven to be great candidates for TAVI. In the below video, Interventional Cardiologist Dr Jonathan White discusses the procedure.
The TAVI Procedure
During the TAVI procedure, a biological (tissue) valve is mounted inside a stent (a circular wire mesh). The stent is then compressed so that it can fit inside a small delivery sheath (tube). The TAVI valve is then delivered to the aortic valve through the sheath, the stent is expanded, and the biological valve begins to operate. In TAVI, the calcified leaflets of the patients’ diseased aortic valve are not removed; instead, the valve pushes the leaflets to the side when the stent is expanded and help to lock the stent in place.
There are multiple options available to operators when performing a TAVI to replace a damaged aortic valve, these include:
- Transfemoral – An incision is made into the femoral artery in the patient’s groin, a delivery sheath is inserted, and the TAVI valve travels upwards through the artery to the aortic valve.
- Transapical – A 5-10cm horizontal incision is made on the left side of the chest below the nipple line to provides direct access to the heart. A delivery sheath is then inserted in the apex of the heart, followed by the TAVI valve.
- Transaortic – A small incision is made at the top of the sternum (breast bone), and the delivery sheath is inserted into the aorta (the large blood vessel that the aortic valve is in), followed by the TAVI valve5.
TAVI Procedure: Step-By-Step
Interventional Cardiologist Dr Gerard Wilkins gives a step by step explanation of the transcatheter aortic valve implantation (TAVI) procedure. A long-tapered sheath travels a wire to the aortic valve. A balloon is used to open up the diseased valve opening. The TAVI valve is guided around the aorta and positioned inside the diseased aortic valve.
 Step 1 of 4
Step 1 of 4
Access to the femoral artery is made through a small incision into the groin. A small radiopaque wire is introduced into the femoral artery and fed into the Aorta. A larger sheath is then introduced into the femoral artery, which allows the introduction of the delivery sheaths with new bio-prosthetic valves in situ.
 Step 2 of 4
Step 2 of 4
The appropriately sized valve is then compressed (downsized) to attach to the delivery catheter, which is ready to be introduced into the femoral artery.
 Step 3 of 4
Step 3 of 4
The delivery catheter is placed in position within the native aortic valve. A balloon is inflated to stretch the size of the diseased valve, then the bio-prosthetic valve is deployed and sits within the damaged native aortic valve. All catheters are then removed from the patient with only the original access catheter left in situ.
 Step 4 of 4
Step 4 of 4
The replaced aortic valve begins to function immediately after being deployed, sitting within the old native valve. Remaining catheters are then removed, and the femoral artery closed as required. A repeat echocardiogram may then be performed to ensure that the replaced valve is functioning effectively.
The Benefits of TAVI
In the below video, Interventional Cardiologist Dr Krys Milburn discusses the benefits of TAVI, including the patient journey, valve types, and recovery time. He also discusses the role of patient frailty, their commodities and quality of life.
TAVI is usually performed in a Cardiac Catheter Laboratory and utilises a minimally invasive approach to replace the diseased aortic valve. Once implanted, the new aortic valve is functional immediately. Benefits of TAVI can include:
- Access for high-risk surgical candidates when previously denied surgical access due to risk6
- Reduction in ICU admission days7
- Faster recovery times compared to SAVR8
- Shorter procedure time compared to SAVR9
- Shorter hospitalisation times10
- TAVI may potentially allow valve-in-valve replacement in the future11
- Less frequent bleeding compared to open surgery9
The Complications of TAVI
All surgical interventions pose an element of risk to the patient. Transcatheter Aortic Valve Implantation (TAVI) complications may include5:
- Degradation or reduced durability/longevity of bio-prosthetic valve
- Bleeding
- Blood vessel complications- rupture/ dissection
- Problems with the replaced valve such as aortic regurgitation and incorrectly sized prosthesis
- Para-valvular leak
- Stroke/ TIA’s
- Arrhythmias – (heart block) which may require permanent pacemakers
- Acute kidney injury
- Heart attack
- Infection
- Death12,13
Balloon Valvuloplasty
Balloon Aortic Valvuloplasty (BAV) has been used as a temporary treatment for aortic stenosis. This procedure is usually performed in a Cardiac Catheter Lab and involves the introduction of a balloon into the diseased aortic valve, the balloon is inflated and then deflated, then removed.
Cardiothoracic Surgeon Mr Indran Ramanathan discusses the consideration for Balloon Valvuloplasty. This treatment option may be considered for “patients who have severe aortic stenosis, but the gradient is very low; we call this low gradient, severe aortic stenosis.”
The principle is to increase the size of the diseased valve, reducing the transaortic valvular pressure, thus relieving symptoms of aortic stenosis for the patient14. This technique may also be used to assess the potential benefits of TAVI prior to a formal TAVI procedure. BAV may be used as a bridge to treatment to allow patients to improve their physical condition prior to a formal aortic valve replacement by either TAVI or SAVR15.
Despite temporarily relieving patient symptoms, restenosis often returns as diseased valve returns to its pre-procedure state. The frequent return of AS symptoms confirm the palliative nature of this treatment option.
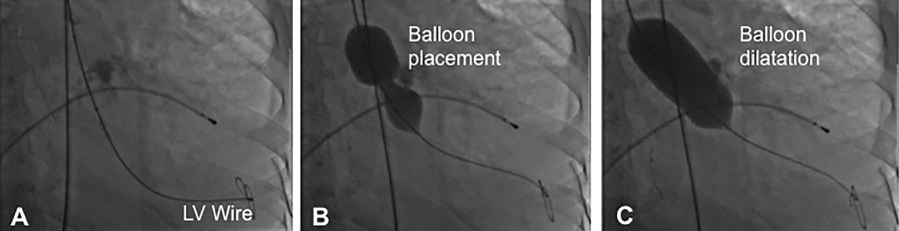
Image 1: Example of a Balloon Valvuloplasty procedure
Patient Disclaimer: All content on the Hope For Hearts site is created and published online for general information purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Please see your doctor if you have any questions or concerns.
Reference
- Mayo Clinic Staff
- National Institute For Health Research
- The DrsWolfson
- Sydney Heart & Lung Surgeons
- Journal of the American College of Cardiology
- Mayo Clinic
- BioMed Central
- BMJ
- The New England Journal of Medicine
- Oxford Academic - European Heart Journal
- Interventional Cardiology Review
- Mayo Clinic
- The Medical Journal of Australia
- BMJ Journals
- Journal of the American College of Cardiology
